RETINA
- RETINA
- INVESTIGATION
- RETINAL PROCEDURES
- DIABETIC RETINOPATHY
- ARMD
- MACULAR HOLE
- MACULAR DEGENERATION
- RETINAL DETACHMENT
- RLP
- ROP
- VITREO RETINAL SURGERY
Understanding the Retina
The human eye functions like a sophisticated camera. The retina plays a central role in the intricate process of vision. Comprising specialized cells, the retina transforms incoming light into electrical signals that are transmitted to the brain. These signals are then interpreted as visual information. This vital organ- the retina is therefore responsible for essential tasks requiring fine vision, such as reading, recognizing faces, and discerning intricate details.
The Macula
The macula is positioned at the heart of the retina. It holds pivotal significance for our daily visual experiences. It is the primary site for straight-ahead vision and view of what lies directly in our line of sight. The health of the macula is of paramount importance for tasks demanding precision.
Essential daily activities like reading, looking at details, and recognizing faces heavily depend on the optimal functioning of the macula. This small but crucial area ensures that we can focus on objects with clarity and perceive fine details. Any compromise in the health of the macula can significantly impact our ability to engage in routine activities that require sharp, detailed vision- this is why, it is necessary to consult a retina specialist if there is even a minor problem here.
Role of the Retina Specialist
Viaan Eye and Retina Centre is the best retina specialist in Gurgaon, particularly renowned for its focus on retina-related services. A retina specialist like Dr. Neeraj Sanduja, equipped with specialized training, can help in the diagnosis and treatment of various retinal conditions.
Importance of Regular Eye Examinations
Regular eye examinations, especially for individuals at risk of retinal disorders, are very important for the early detection of retinal issues. This is why it is necessary to get your eyes checked by a retina specialist if are prone to frequent eye problems, are nearing old age, or have any other disease like diabetes or hypertension.
The macula, being a delicate part of the retina, requires a thorough examination to identify and address problems and come up with a suitable diagnosis. Viaan Eye and Retina Centre prioritizes comprehensive eye checks. We utilize advanced diagnostic technologies to catch even the most minor issues before they escalate.
Viaan Eye and Retina Centre – Best retina specialist in Gurgaon
Viaan Eye and Retina Centre in Gurgaon boasts a team of highly skilled retina specialists under the extremely able leadership of Dr. Neeraj Sanduja. These experts handle a range of different retinal conditions, from common issues like diabetic retinopathy to more complex cases such as retinal detachment. Their expertise lies not only in diagnosis but also in providing personalized treatment plans according to each patient’s unique needs.
Cutting-Edge Technology for Precision Care
The Viaan Eye and Retina Centre as the best retina specialist in Gurgaon utilizes advanced diagnostic technologies to assess the health of the retina accurately. This ensures that even the most subtle and unnoticeable issues are identified early, allowing for timely interventions. This can significantly impact the preservation and enhancement of your vision.
A healthy macula is crucial for tasks involving fine vision such as reading, recognizing faces and distinguishing things. The area surrounding the macula helps in mobility and in seeing from the ‘corner’ of the eye. The retina is connected to the brain by the optic nerve. In front of the retina is the vitreous cavity, which is filled with a gel-like substance, called the vitreous.
INVESTIGATIONS IN RETINAL DISEASES
- FUNDUS FLUORESCEIN ANGIOGRAPHY
A self-explanatory consent form, which explains the side effects in detail, is provided to the patients by the retina specialist. Consent is required before the procedure. Patients can have a light meal before undergoing the procedure and must be accompanied by a family member.
Eye drops are administered by the retina specialist to enlarge the pupils — this takes approximately 30-40 minutes. The patient is then asked to sit still in front of the camera while a series of colour photographs of the eyes are taken by the retina specialist. An injection (contrast) is then injected and more photographs are taken by the retina specialist.
The test takes approximately 10-15 minutes.
It is a very safe procedure and serious side effects are uncommon. However, there is a rare possibility that a patient may react to the contrast. Some patients may experience slight nausea after the dye injection, but the feeling usually passes quickly. Either way, Viaan Eye and Retina Centre as the best retina specialist in Gurgaon takes proper measures to care for the patient in case of any side effects.
Patients who are allergic to the dye can develop itching and a skin rash. These symptoms generally respond quickly to medications such as anti-allergics or steroids.
There is also a possibility of the dye going into the skin at the injection site, this may cause some discomfort or discolouring of the skin for several days. The fluorescein dye turns the patient’s urine orange and may slightly discolour the skin as well for a brief period.
- ULTRASONOGRAPHY OF THE POSTERIOR SEGMENT
A thick jelly is placed on the ultrasound probe by the retina specialist, which is then gently placed on the eye over the lid. It is a safe and painless procedure, no X-ray exposure occurs in this test. The retina specialist uses these echo pictures to arrive at a diagnosis, the probable future health of your eye, and a treatment plan. However, the test only reveals the structure of the inside of the eye.
- OPTICAL COHERENCE TOMOGRAPHY (OCT)
Optical coherence tomography is a non-invasive imaging test, which uses light waves to take cross-section pictures of patients’ retina.
With OCT, the retina specialist can see each of the retina’s distinctive layers. This allows mapping and measuring retinal thickness. These measurements help with diagnosis. OCT also guides treatment for retinal diseases, like age-related macular degeneration (AMD), diabetic eye disease, and macular oedema.
The retina specialist may or may not put dilating eye drops. These drops widen the pupil and make it easier to examine the retina.
The patient sits in front of the OCT machine and rests their head and chin on a support to keep them motionless. The retina specialist then scans the eye without touching it. Scanning takes about 5 to 10 minutes.
OCT is often used to evaluate disorders of the optic nerve as well. The OCT exam helps the retina specialist see changes to the fibres of the optic nerve. For example, it can detect changes caused by glaucoma.
OCT relies on light waves. It cannot be used with conditions that interfere with light passing through the eye. These conditions include dense cataracts or significant bleeding in the vitreous.
- OPTICAL COHERENCE TOMOGRAPHY ANGIOGRAPHY (OCTA)
This test takes pictures of the blood vessels in and under the retina. OCTA is like fluorescein angiography, but is a much quicker test and does not use a dye (dyeless angiography). It can be safely done by the retina specialist in patients allergic to fluorescein dye and with renal disease (where dye/ contrast is contraindicated)
OCT and OCTA help the retina specialist diagnose many eye conditions, including:
– macular hole
– macular pucker
– macular edema
– age-related macular degeneration
– Central serous retinopathy
– diabetic macular edema
– abnormal blood vessels within/ underneath the retina
– blood vessel blockage
RETINAL PROCEDURES
- INTRAVITREAL INJECTIONS
a) Anti-VEGF treatment
Anti-VEGF (anti-vascular Endothelial Growth Factor) injections are a group of medicines administered by the retina specialist which reduce new blood vessel growth or oedema (swelling). They can be used to treat several eye conditions which cause new blood vessel growth or swelling under the macula area of the retina.
Currently, anti-VEGF treatment is used by a retina specialist for:
- ‘wet’ Age-related macular degeneration (AMD)
- Diabetic maculopathy
- Macular oedema caused by retinal vein occlusion.
- Myopic Choroidal Neovascularisation.
- Retinopathy of Prematurity. (ROP)
New blood vessel growth and macular oedema can also occur in other retinal conditions, so Dr. Neeraj Sanduja, the best retina specialist in Gurgaon says that in the future anti-VEGF medications may be used in a wider range of situations.
Anti-VEGF treatments are given by an injection into the white portion of the eye and work by reducing the growth of new blood vessels and the oedema (swelling). Doing this can reduce the risk of scarring and damage to the retina caused by these new vessels, which in turn can help to avoid further sight loss and for some people cause an improvement in vision.
Depending on the condition of the patient, the retina specialist performs tests to decide whether treatment with antiVEGFs is required.
After examining the eye, the retina specialist may undertake further tests to have a clearer picture of the patient’s eye and symptoms.
Procedure
Anti-VEGF drugs are given as an injection into the vitreous (the jelly-like substance inside the eye). The injection is given through the white of the eye (the sclera). The injection needs to be given by the retina specialist in a sterile way in an operating theatre.
The needle used for the injection is small and short and the injection itself only takes a few seconds. The patients have had an anaesthetic drop in their eye, before the procedure, so the injection feels like a small point of pressure on the eye.
After the injection, vision may be blurry for several hours because of the dilating eye drops; this should improve by the next day or the day after. The white of the eye may get red after the injection for a few days. Black swirls in the vision may be noticed for a few weeks (this is the drug floating in the vitreous gel). The eye usually feels comfortable by the next day. Some eye drops are given by the retina specialist for a few days after the injection to prevent an infection.
The different AntiVEGFs available are:
- ACCENTRIX (RANIBIZUMAB)
- EYLEA (AFLIBERCEPT)
- PAGENAX (BROLUCIZUMAB)
- AVASTIN (Bevacizumab, off-label use)
- RAZUMAB, RANIEYES, OCEVA ( RANIBIZUMAB BIOSIMILARS)
b) Steroids
Intravitreal steroids are used in some eyes with diabetic retinopathy, retinal vein occlusion and uveitis. Steroids help to reduce fluid leakage associated with these disorders.
The commonly used steroid is Dexamethasone Implant (Ozurdex), which is injected by the retina specialist in the vitreous cavity just like any anti-VEGF drug.
c) Antibiotics
Antibiotic, antifungal and antiviral drugs are injected into the vitreous cavity by the retina specialist to treat patients with infections in the eye such as endophthalmitis and retinitis.
DIABETIC RETINOPATHY
Diabetic retinopathy is a complication that affects the eyes and can develop in anyone who has type 1 or type 2 diabetes. It’s caused by damage to the blood vessels of the retina.
Dr. Neeraj Sanduja, the best retina specialist in Gurgaon says that in its early stages, diabetic retinopathy usually causes no symptoms. As the disease progresses, one might develop:
- Spots or dark strings floating in the vision (floaters)
- Blurred vision
- Fluctuating vision
- Dark or empty areas in the vision
- Vision loss
In later stages, it can even lead to blindness. Thus regular dilated retina evaluations by a retina specialist in diabetic patients can pick up the disease in its early stages and prevent severe vision loss.
The longer one has diabetes and the less controlled one’s blood sugar is, the more likely is he/she to develop diabetic retinopathy.
Risk factors
Anyone who has diabetes can develop diabetic retinopathy. The risk of developing the eye condition can increase as a result of:
- Having diabetes for a long time
- Poor control of blood sugar level
- High blood pressure
- High cholesterol
- Pregnancy
- Tobacco use
- Anaemia, compromised renal status
There are two types of diabetic retinopathy:
- Early diabetic retinopathy. In this more common form — called nonproliferative diabetic retinopathy (NPDR) — new blood vessels aren’t growing (proliferating).
In nonproliferative diabetic retinopathy (NPDR), a retina specialist sees that the walls of the blood vessels in the retina weaken causing leakage of fluid and blood into the retina.
NPDR can progress from mild to severe as more blood vessels become blocked.
Sometimes retinal blood vessel damage leads to a buildup of fluid (oedema) in the centre portion (macula) of the retina. If macular oedema decreases vision, treatment in the form of intravitreal injections/ laser by a retina specialist is required to prevent permanent vision loss.
- Advanced diabetic retinopathy. Diabetic retinopathy can progress to this more severe type, known as proliferative diabetic retinopathy (PDR). In this type, damaged blood vessels close off, causing the growth of new, abnormal blood vessels in the retina. These new blood vessels are fragile and can leak into the clear, jellylike substance that fills the centre of the eye (vitreous). (Vitreous Haemorrhage) In this case, immediate attention is needed and it is recommended that you visit the best retina specialist in Gurgaon
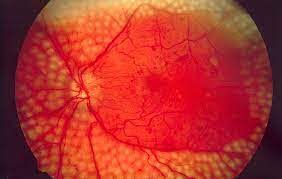
PROLIFERATIVE DIABETIC RETINOPATHY (PDR)
PDR WITH VITREOUS HAEMORRHAGE
Eventually, scar tissue from the growth of new blood vessels can cause the retina to detach from the back of the eye. (Tractional Retinal Detachment)
PDR WITH TRACTIONAL RETINAL DETACHMENT
If the new blood vessels interfere with the normal flow of fluid out of the eye, pressure can build in the eyeball. This build-up can damage the nerve that carries images from the eye to the brain (optic nerve), resulting in glaucoma. (Neovascular Glaucoma)
Prevention
Regular eye exams by a retina specialist, good control of blood sugar and blood pressure, and early intervention by the best retina specialist in Gurgaon for vision problems can help prevent severe vision loss.
- Regular monitoring and good control of blood sugar levels.
- Ask your retina specialist about a glycosylated haemoglobin test. The glycosylated haemoglobin test, or haemoglobin A1C test, reflects the average blood sugar level for the two- to three-month period before the test. For most people with diabetes, the A1C goal is to be under 7%.
- Keeping blood pressure and cholesterol under control.
- Avoid smoking/ or use of other types of tobacco
- Pay attention to vision changes
TREATMENT
- Injections: anti-VEGFs/ steroid:
These medications when injected in the back of the eye by a retina specialist, help reduce swelling of the macula, slowing vision loss and perhaps improving vision. Multiple such injections are needed depending on the severity of one’s Diabetic Retinopathy and control.
- Laser Treatment
Laser is used to help seal off leaking blood vessels (FOCAL LASER). This can reduce swelling of the retina.
The laser can also help shrink blood vessels (PANRETINAL PHOTOCOAGULATION/ PRP LASER) and prevent them from growing again. This is done in multiple sittings. Sometimes more than one treatment is needed as recommended by the retina specialist
LASERED DIABETIC RETINA (AFTER PRP LASER)
- Vitrectomy
With advanced PDR, (Vitreous Haemorrhage or Tractional Retinal Detachment), surgery called vitrectomy (Pars Plana Vitrectomy/ MicroIncision Vitrectomy Surgery) is needed.
AGE RELATED MACULAR DEGENERATION (AMD)
Age-related macular degeneration (AMD) is a problem where a part of the retina called the macula is damaged due to ageing. This condition requires a medical diagnosis by a retina specialist.
AMD is very common and is a leading cause of vision loss in people 50 years or older.
With AMD there is a loss of central vision, fine details, and near vision, with sparing of peripheral (side) vision.
Two Types of AMD
- Dry AMD
This form is quite common. About 80% (8 out of 10) of people who have AMD have the dry form. Dry AMD is when parts of the macula get thinner with age and tiny clumps of protein called drusen grow. There is a slow loss of central vision. There is no way to treat dry AMD yet but consultation with a retina specialist may help you slow down the progression of the problem.
DRY AGE-RELATED MACULAR DEGENERATION (DRUSENS)
DRY AGE-RELATED MACULAR DEGENERATION (GEOGRAPHIC ATROPHY)
- Wet AMD
This form is less common but much more serious and requires more careful attention by the retina specialist. Wet AMD is when new, abnormal blood vessels grow under the retina. These vessels may leak blood or other fluids, causing scarring of the macula. There is faster central vision loss with wet AMD than with dry AMD.
Many people don’t realize they have AMD until their vision is very blurry. This is why it is important to have regular visits to a retina specialist, who can look for early signs of AMD before any vision loss happens.
WET AGE-RELATED MACULAR DEGENERATION
Age-Related Macular Degeneration Treatment
Dry AMD Treatment
Right now, there is no way to treat the dry form of AMD. However, people with lots of drusen or serious vision loss might benefit from taking a certain combination of nutritional supplements.
Wet AMD Treatment
To help treat wet AMD, there are medications called anti-VEGF drugs. Anti-VEGF treatment by a retina specialist helps reduce the number of abnormal blood vessels in the retina and slows any leaking from blood vessels.
MACULAR HOLE
It is a full-thickness defect in the macula (the vision-forming portion of the retina)
The most common symptom of a macular hole is a gradual decline in the central (straight-ahead) vision of the affected eye. This is when you should get yourself tested by a retina specialist. This can occur as:
– Blurring
– Distortion (straight lines appearing wavy)
– A dark spot in the central vision
If you have any such symptoms, you should surely consider consulting a retina specialist. Viaan Eye and Retina Centre is the best retina specialist in Gurgaon. The degree to which vision is affected depends on the size of the macular hole, as well as the stage of its development.
Macular hole commonly affects people over the age of 55 and most often occur in women. The vast majority of cases develop spontaneously without an obvious cause. For this reason, there is currently no effective way to prevent its formation and development. If a macular hole develops in one eye, there is a 5% to 15% risk of one developing in the other eye.
Diagnostic Testing
Clinical examination by a retina specialist is followed by Optical Coherence Tomography
OCT IN FULL THICKNESS MACULAR HOL
Optical coherence tomography (OCT) is the current gold standard in the diagnosis, staging, and management of macular holes at Viaan Eye and Retina Centre, the best retina specialist in Gurgaon.
Treatment and prognosis
The treatment for a full-thickness macular hole is surgical, which is Vitrectomy surgery, in which the vitreous gel is removed to stop it from pulling on the retina, following which a gas bubble is placed in the eye to gently hold the edges of the macular hole closed until it heals.
The patient is asked by the retina specialist to maintain a face-down position up to 2 weeks, depending on the characteristics of the macular hole.
Vitrectomy at Viaan Eye and Retina centre under the able guidance of Dr Neeraj Sanduja, the best retina specialist in Gurgaon has a success rate of over 90%, with patients regaining some or most of their lost vision, with potential complications being cataract formation, retinal detachment, infection, glaucoma, bleeding, and re-opening or persistence of the macular hole (less than 10% of cases)
OCT of a patient before and after Vitrectomy surgery of a Macular Hole
RETINAL LASER PHOTOCOAGULATION
It is an OPD procedure done by a retina specialist used to treat a number of retinal conditions, including
– retinal holes or tears, (Barrage Laser)- to seal a retinal tear to prevent the development of a retinal detachment, a potentially blinding condition.
– proliferative diabetic retinopathy, (Pan Retinal Photocoagulation / PRP Laser) – to seal or destroy leaking blood vessels to prevent further retinal damage and preserve vision
– macular edema (Focal Laser)
– retinal vein occlusion. (Sectoral PRP Laser)
– and Central Serous ChorioRetinopathy (Focal Laser)
The laser procedure works by creating small areas of scar tissue that can seal off a tear or leaking blood vessels. It can also slow the growth of abnormal blood vessels (neovascularization) in the eye.
The procedure cannot typically restore vision that is already lost, but it can reduce the risk of future vision loss. This is why it is crucial to get checked by the best retina specialist at Viaan Eye and Retina Centre in Gurgaon at the earliest!
MACULAR DEGENERATION
What is Macular Degeneration?
Macular degeneration is also known as age-related macular degeneration (AMD). It is a progressive eye condition that affects the macula in the retina. The macula is the central part of the retina responsible for sharp, central vision. This condition is usually caused by old age and progressively increases as a person grows older. This impacts the ability of the affected person to see fine details. In such a case, it is best to consult a retina specialist.
Causes of Macular Degeneration:
The main cause of macular degeneration is the process of ageing. However, some factors can increase the risk of the onset of macular degeneration in a person. A retina specialist will tell you that these factors are inclusive of genetics, smoking, obesity, and a diet low in nutrients like vitamins C and E, zinc, and carotenoids.
Symptoms and When to Visit the Doctor:
One of the main concerns of Macular Degeneration is that in the early stages, it may not exhibit any noticeable symptoms. That is why it is often overlooked and this causes the condition to worsen! But as the condition progresses, the retina specialist says that individuals may experience:
– Blurred or distorted vision.
– Difficulty in recognizing faces.
– Straight lines appearing wavy or crooked.
If you notice any such changes in your vision, it is best to check with a retina specialist. Especially if you fall within the high-risk categories, it’s crucial to visit the best retina specialist in Gurgaon promptly. To ensure the health of your eye, regular eye check-ups become even more critical with age, helping the retina specialist detect and address potential issues early.
Treatment:
While people say that there is no cure for complete macular degeneration, certain treatments and lifestyle adjustments can help you manage the condition and slow down its progression. These include:
– Dietary supplements containing vitamins like Vitamin A, E, and K and minerals that support eye health.
– Anti-VEGF drugs can be administered by the retina specialist. These are injected into the eye to inhibit the growth of abnormal blood vessels slowing down the process of Macular Degeneration
– Laser therapy can be done by an expert retina specialist to destroy abnormal blood vessels.
Early detection and proactive management are key components of effective treatment and this can be achieved only through timely consultation with a retina specialist.
Expected Procedures:
- Comprehensive Eye Examination: The retina specialist will conduct a thorough eye exam, including:
– a visual acuity test,
– dilated eye exam, and
– imaging tests like OCT or fluorescein angiography
This helps the retina specialist assess the extent of macular degeneration and suggest the appropriate measures.
- Treatment Administration: Depending on the severity, treatment procedures such as anti-VEGF injections or laser therapy may be recommended by the retina specialist.
- Ongoing Monitoring: Macular degeneration is a progressive condition. This is why it is highly required to be regularly monitored by a retina specialist to track changes and adjust the treatment plan accordingly.
Viaan Eye and Retina Centre as the best Retina Specialist in Gurgaon:
Viaan Eye and Retina Centre in Gurgaon stands out as the best Retina Specialist in Gurgaon for specialized care in retinal conditions, including macular degeneration. With a team of experienced retina specialists, led by the best Retina Specialist in Gurgaon- Dr. Neeraj Sanduja, Viaan Eye and Retina Centre is the name you can trust!
Viaan Eye and Retina Centre uses advanced diagnostic technologies like OCT and a commitment to personalized treatment plans. This ensures comprehensive and effective care for individuals dealing with macular degeneration. The unmatched expertise, coupled with a patient-centric approach, makes them the best retina specialist for those seeking specialized care in Gurgaon.
RETINAL DETACHMENT
What Is a Detached Retina?
What Is a Detached Retina?
A detached retina is when the retina lifts away from the back of the eye. The retina does not work when it is detached, making vision blurry. A detached retina is a serious problem and needs immediate attention by a Retina specialist so that the problem is treated and measures can be taken to prevent the further loss of vision.
How Does the Retina Detach?
With ageing, the vitreous in the eyes starts to shrink and get thinner. As the eye moves, the vitreous moves around on the retina without causing problems. But sometimes, as the vitreous shrinks, it may pull hard enough to cause a tear in the retina. When that happens, fluid can pass backwards through the tear and lift (detach) the retina.
RHEGMATOGENOUS RETINAL DETACHMENT (RRD)
Who Is at Risk for Retinal Detachment?
One is more likely to have a detached retina if he/she
- needs glasses to see far away (nearsightedness or myopia)
- has had cataract, glaucoma, or other eye surgery
- takes glaucoma medications that make the pupil small (like pilocarpine)
- had a serious eye injury(trauma)
- had a retinal tear or detachment in the other eye
- has family members who have had retinal detachment
- have weak areas in the retina (seen by a retina specialist during a dilated retinal exam)
Such people should look out for the early signs of a retina detachment and consult a Retina specialist at once if symptoms persist.
Early Signs of a Detached Retina
- Seeing flashing lights all of a sudden, perceived as sparkling lights in dim light
- Noticing many new floaters at once. These can look like specks, lines or cobwebs in the field of vision.
- A shadow appearing in the peripheral (side) vision.
- A grey curtain covering part of the field of vision.
If you are experiencing any of these symptoms, it is highly recommended that you visit the Viaan Eye and Retina Centre and get yourself checked by the best Retina specialist in Gurgaon
Floaters
Peripheral field loss
How Is a Detached Retina Diagnosed?
The Retina specialist will put drops in the eyes to dilate (widen) the pupil and will look through a special lens and a head-mounted instrument to check the retina. Sometimes an Ultrasound of the back of the eye may be needed to diagnose the detachment.
ULTRASOUND OF RETINAL DETACHMENT
How Is a Detached Retina Treated?
Surgery is done by a Retina specialist to repair a detached retina. Kindly refer to the Retinal Surgery Section.
RETINAL LASER PHOTOCOAGULATION
It is an OPD procedure done by a retina specialist used to treat several retinal conditions, including
– retinal holes or tears, (Barrage Laser)- to seal a retinal tear to prevent the development of a retinal detachment, a potential blinding condition.
– proliferative diabetic retinopathy, (Pan Retinal Photocoagulation / PRP Laser) – to seal or destroy leaking blood vessels to prevent further retinal damage and preserve vision
– macular edema (Focal Laser)
– retinal vein occlusion. (Sectoral PRP Laser)
– and Central Serous ChorioRetinopathy (Focal Laser)
The laser procedure done by a retina specialist works by creating small areas of scar tissue that can seal off a tear or leaking blood vessels. It can also slow the growth of abnormal blood vessels (neovascularization) in the eye.
The procedure cannot typically restore vision that is already lost, but it can reduce the risk of future vision loss. This is why, it is highly recommended that you visit Viaan Eye and Retina Centre, the best retina specialist in Gurgaon to prevent any further vision loss.
RETINOPATHY OF PREMATURITY
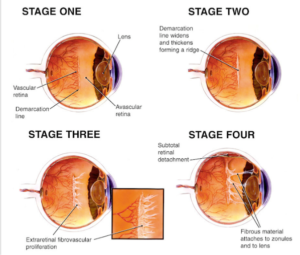
What is ROP?
Retinopathy of Prematurity (ROP) is a potentially serious eye condition that primarily affects premature infants. It occurs when the blood vessels in the retina, the light-sensitive tissue at the back of the eye, do not develop properly. This condition may seem very scary for the parents of the little infant but consulting a good retina specialist like Dr. Neeraj Sanduja can alleviate some of your worries.
What are the main causes of ROP?
The main cause of ROP is the immature development of blood vessels in the retina, which is common in premature infants. Factors such as:
– low birth weight,
– premature birth, and
– exposure to high levels of oxygen during neonatal care
Contribute to the risk of developing ROP.
Symptoms and When to Visit the Doctor:
ROP often presents itself in an infant with no visible symptoms in its early stages. It is necessary to keep monitoring premature infants, especially those with low birth weight. If there are signs of abnormal blood vessel development, such as a white appearance in the pupil or abnormal eye movements, it is absolutely essential to bring this to the attention of a retina specialist. Regular eye exams by the best retina Specialist in Gurgaon for premature infants are recommended to detect ROP early.
What are the Treatments available for ROP?
Retina specialist, Dr. Neeraj Sanduja, says that the severity of ROP determines the course of treatment. Mild cases of ROP may resolve on their own as the infant’s eyes continue to develop. However, there is a need to constantly monitor the progress. However, more advanced cases may require intervention by a retina specialist to prevent vision loss. Treatment options include laser therapy to stop abnormal blood vessel growth and, in some cases, injections of medication into the eye. You can consult Dr. Neeraj Sanduja and his team, the best retina Specialist in Gurgaon to get more clarity on the position.
Expected Procedures for ROP:
Regular eye examinations by a retina specialist for premature infants involve the use of specialized instruments to examine the retina. The retina specialist will carefully assess the blood vessels, ensuring that if there are any signs of ROP, they are detected early. In cases requiring treatment, laser therapy or injections may be recommended by the retina specialist to preserve the infant’s vision.
Viaan Eye and Retina Centre as the Best Retina Specialist in Gurgaon:
Viaan Eye and Retina Centre, recognized as the Best Retina Specialist in Gurgaon, is dedicated to providing specialized care for retinal conditions, including Retinopathy of Prematurity. The centre has a team of experienced retina specialists under Dr. Neeraj Sanduja- the best retina specialist in Gurgaon– who understands the unique needs of premature infants. Using state-of-the-art diagnostic tools and treatment modalities, Viaan Eye and Retina Centre ensures comprehensive care tailored to each patient and each condition.
The retina specialists at Viaan Eye and Retina Centre prioritize early detection and intervention. They prioritize and understand the critical importance of preserving the vision of premature infants because this affects them for a lifetime. Viaan Eye and Retina Centre is a centre you can trust!
Vitreo Retinal Surgery
As the name implies, this delicate surgery (done by a retina specialist) takes place where the gel-like vitreous and light-sensitive layer inside the eye (retina) is found.
Common Indications for Vitrectomy
- Diabetic vitreous hemorrhage.
- Retinal detachment – Rhegmatogenous (secondary to a retinal break) or Tractional
- Epiretinal membrane.
- Macular hole.
- Proliferative vitreoretinopathy.
- Endophthalmitis.
- Intraocular foreign body removal.
- Retrieval of lens nucleus following complicated cataract surgery.
- Retrieval of a dropped Intraocular Lens.
VARIOUS TREATMENT OPTIONS
Retinal holes or breaks are treated by a retina specialist with laser photocoagulation (a form of heat therapy) or cryopexy (a freeze treatment) as an outpatient procedure. During laser treatment, the retina specialist places dot-like burns around the break to “weld/ seal” the break. In Cryopexy the area around the break is frozen and it helps seal the break.
Retinal Detachments are treated with surgery viz scleral buckling and complex vitreoretinal surgery (MicroIncision Vitrectomy) involving the use of Silicone oil or gases.
In scleral bucking, a silicon band is anchored with stitches around the eyeball to gently push the wall of the eye against the detached retina.
In a vitrectomy, three tiny incisions are made by the retina specialist in the white of the eye to create openings for the various instruments that are inserted inside the eye, that do not usually require placement of stitches afterwards (i.e. micro-incision sutureless surgery). The instruments that pass through these incisions include
- Light pipe, which serves as a microscopic, high-intensity flashlight for use within the eye.
- Infusion port, used to replace fluid in the eye with a saline solution and to maintain proper eye pressure.
- Vitrector, or cutting device, that removes the eye’s vitreous gel in a slow, controlled fashion. It protects the delicate retina by reducing traction/ pull while the vitreous gel is removed.
Once the vitreous gel is removed, the retina specialist replaces it with silicone oil/ gas to keep the retina in place.
What To Expect?
Bleeding, infection, progression of cataracts and retinal detachment are potential problems after any retinal surgery, but these complications are relatively unusual.
With modern vitreoretinal instrumentation used by Viaan Eye and Retina Centre- the best retina specialist in Gurgaon, around 90 per cent of cases with a retinal detachment can be successfully treated. Visual results are good if the retinal detachment is repaired before the macula (the centre region of the retina responsible for fine, detailed vision) detaches. Thus, it is important to contact your retina specialist in time when you notice any flashes or floaters or a curtain in the field of vision.
Surgery is generally performed under local anaesthesia (i.e. the patient is awake but the eye is anesthetized via local retrobulbar/ peribulbar lidocaine/marcaine). This allows for the fastest and safest surgery with essentially no risk systematically.
Depending on the type of condition, the surgery can last anywhere between 30-90 minutes. Once the surgery is completed, the patient’s eye is patched until their post-op visit which is usually within 24 hours following surgery.
At the first postoperative visit, the patch is removed and instructions including the use of eye drops are given by the retina specialist. Following surgery, often special positioning (e.g. face down) is required for the retinal condition to be managed.
Vision following surgery is hindered for up to 6 weeks if gas is utilized. There is typically very minor discomfort following surgery lasting 24-48 hours. It is extremely rare to have severe pain following surgery; if that happens or there is any vision loss, patients are advised to contact the retina specialist immediately.
If Silicone oil is injected, the patient requires a second surgery for its removal from the eye.



